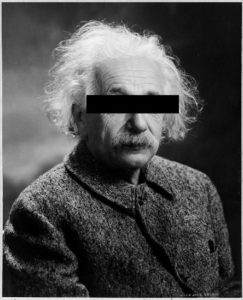
Some of you may remember a fashion magazine that ran a special feature called Do’s and Don’ts. People unfortunate enough to be called out as a “don’t” were wearing not only some hideous outfit, but they also sported a thin black bar over their eyes.
So what’s the problem with that? Well the main thing is, those black bars don’t protect identity. For example (and I am not condemning this fashion choice, by the way), how anonymous is the man in the image?
Publishing Illustrative Content and Protecting Patients’ Rights
Editors who work with clinical content, especially case reports, are familiar with the challenges of balancing patient confidentiality with the dissemination of important clinical information. Photographs are useful to show unique manifestations of a condition, to illustrate new techniques or procedures, and to help clinicians quickly visualize anatomic landmarks or other important details.
Until the late 1980s, placing black bars over the eyes in photographs was often accepted as a way to protect patient identity. However, some journals discontinued this practice when it became apparent that bars across the eyes do not preserve confidentiality. The International Committee of Medical Journal Editors recommendations on the protection of research participants notes that “masking the eye region in photographs of patients is inadequate protection of anonymity.”1
But the risk of patient identifiability is not limited to black bars over the eyes. Individuals can be identified in photographs that may have been cropped to remove faces but reveal other identifying features (e.g., hair, scars, moles, tattoos, clothing).2
Another figure type that can be revealing is not pictorial—it’s a pedigree. While pedigrees may not be as readily identifiable as a patient’s face, they can pose a risk to patient (and family member) confidentiality, especially when rare diseases are described.
Figures are not the only concern. Patients have recognized descriptions of themselves in articles without accompanying photographs, just based on text descriptions (not only in clinical reports but also narratives) or demographic and clinical data in a table. And the need to protect patient identity also extends to multimedia, such as audio interviews or videos.
So What’s an Editor to Do?
To protect a patient’s right to privacy, nonessential identifying data (e.g., sex, age, race/ethnicity, occupation, and location of treatment) can be removed from a manuscript, unless clinically or epidemiologically relevant or important. However, omitting certain details may be problematic (e.g., age or occupation may be important to future epidemiologic investigations). More important, authors and editors should not alter or falsify details in case descriptions to secure anonymity because doing so may introduce false or inaccurate data into the medical literature.2
Photographic images can be cropped as long as important clinical information is not lost and no identifying details remain (e.g., jewelry, tattoos). Even seemingly insignificant characteristics can compromise patient confidentiality—it’s not just that a patient’s coworker or neighbor might recognize them; the threshold for identifiability is the individual person (i.e., if the patient can recognize themselves). In situations in which patient anonymity cannot be guaranteed, attempts to deidentify clinical photographs and related text description should be abandoned.3
The ideal approach, of course, is to have written permission from the patient (or parent/legal guardian in the case of minors) depicted or described for publication of their information. Such consent should include an opportunity for the patient to read the manuscript before publication or waive the right to do so. Many journals have their own consent forms that they require for this. Although institutions often obtain consent from patients to use such information obtained in a medical encounter or research for “educational purposes or publication,” such consent does not always cover publication in journals or online.2 When this permission is obtained, it should be noted in the published article.1
It may be tempting to get around these thorny issues by fabricating patients. However, authors should not “invent” patients and present these as actual cases. If a fictionalized or hypothetical case is presented for educational purposes, this should be indicated to readers as a “hypothetical case” or by providing a prominent disclaimer in the article.2
The bottom line: only those details essential for understanding and interpreting a specific report should be provided. Editors should carefully weigh patient confidentiality on a case-by-case basis, including decisions to remove extraneous detail or requests to authors to secure patient permission. The completion of a specific permission form for clinical photographs and other identifying material may seem like a burden, but it serves to protect the interests of all involved: patients, authors, and journals.
References and Links
- International Committee of Medical Journal Editors. Protection of research participants. [accessed February 24, 2021]. http://www.icmje.org/recommendations/browse/roles-and-responsibilities/protection-of-research-participants.html.
- American Medical Association (AMA). Consent for identifiable patients. In: Christiansen S, Iverson C, Flanagin A, et al, editors. AMA Manual of Style. 11th ed. Chicago, IL: AMA. [accessed March 9, 2021]. https://www.amamanualofstyle.com/view/10.1093/jama/9780190246556.001.0001/med-9780190246556-chapter-4-div2-150
- Robinson JK, Bhatia AC, Callen JP. Protection of patients’ right to privacy in clinical photographs, video, and detailed case descriptions. JAMA Dermatol. 2014;150(1):14–16. https://doi.org/10.1001/jamadermatol.2013.8605.
Stacy L Christiansen, MA, is Managing Editor, JAMA, and Chair, AMA Manual of Style committee.
